Table of Contents
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. While the exact cause of depression is not fully understood, research suggests that neurochemical imbalances in the brain play a significant role in its development and progression. In this comprehensive guide, we’ll explore the science behind depression, focusing on the role of neurochemical imbalances and how they contribute to the symptoms of this debilitating disorder.
Introduction to Depression
Depression is more than just feeling sad or down occasionally; it’s a persistent and pervasive feeling of sadness, hopelessness, and despair that significantly impacts a person’s quality of life. Symptoms of depression can vary widely from person to person but may include persistent feelings of sadness or emptiness, loss of interest or pleasure in activities once enjoyed, changes in appetite or weight, difficulty sleeping or oversleeping, fatigue or low energy, feelings of worthlessness or guilt, and difficulty concentrating or making decisions.
Neurochemistry of Depression
Neurochemistry refers to the chemical processes and neurotransmitters that occur within the brain. Neurotransmitters are chemical messengers that transmit signals between nerve cells, or neurons, in the brain. These neurotransmitters play a crucial role in regulating mood, emotion, cognition, and behavior. Several neurotransmitters have been implicated in the development of depression, including serotonin, dopamine, norepinephrine, and gamma-aminobutyric acid (GABA).
Serotonin
Serotonin is often referred to as the “feel-good” neurotransmitter because it helps regulate mood, happiness, and anxiety. Low levels of serotonin have been linked to depression, and many antidepressant medications work by increasing the availability of serotonin in the brain. However, the relationship between serotonin and depression is complex, and researchers continue to investigate how alterations in serotonin function contribute to depressive symptoms.
Dopamine
Dopamine is another neurotransmitter involved in mood regulation, reward, motivation, and pleasure. Like serotonin, imbalances in dopamine levels have been implicated in depression. Some research suggests that individuals with depression may have reduced dopamine activity in certain areas of the brain associated with motivation and reward processing. This may contribute to symptoms such as anhedonia, or the inability to experience pleasure from activities once enjoyed.
Norepinephrine
Norepinephrine, also known as noradrenaline, is involved in the body’s stress response and plays a role in regulating mood and arousal. Dysregulation of norepinephrine levels has been observed in individuals with depression, particularly those with symptoms of fatigue, low energy, and apathy. Medications that increase norepinephrine activity in the brain, such as norepinephrine reuptake inhibitors (NRIs), are sometimes used to treat depression.
Gamma-Aminobutyric Acid (GABA)
GABA is the primary inhibitory neurotransmitter in the brain, meaning it helps reduce the activity of neurons and promote relaxation and calmness. Imbalances in GABA function have been implicated in various mood and anxiety disorders, including depression. Some research suggests that individuals with depression may have reduced GABA levels or impaired GABAergic neurotransmission, which could contribute to symptoms of anxiety and dysphoria.
The Role of Neurochemical Imbalances in Depression
While the precise mechanisms underlying depression remain unclear, it’s believed that neurochemical imbalances disrupt the normal functioning of neural circuits involved in mood regulation and emotional processing. These imbalances can result from a combination of genetic, biological, psychological, and environmental factors, including:
- Genetics: Family history of depression or other mood disorders may increase the risk of developing depression, suggesting a genetic predisposition.
- Brain Structure and Function: Structural and functional abnormalities in certain regions of the brain, such as the prefrontal cortex, amygdala, and hippocampus, have been observed in individuals with depression.
- Hormonal Changes: Fluctuations in hormones, such as cortisol (the stress hormone) and thyroid hormones, may contribute to alterations in neurotransmitter function and mood regulation.
- Stressful Life Events: Trauma, abuse, loss, or other stressful life events can trigger depression in susceptible individuals by disrupting neurochemical balance and activating the body’s stress response system.
Treatment Approaches for Depression
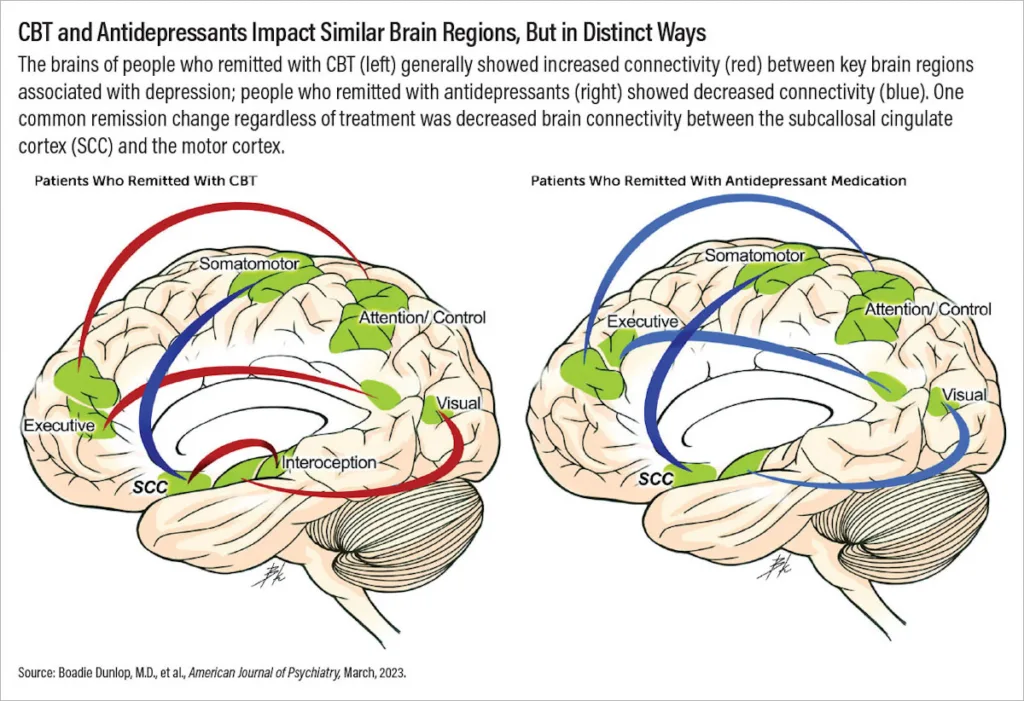
Treatment for depression typically involves a combination of psychotherapy, medication, lifestyle changes, and other supportive interventions. Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and others, are commonly prescribed to help restore balance to neurotransmitter systems implicated in depression. These medications work by increasing the availability of neurotransmitters such as serotonin and norepinephrine in the brain.
In addition to medication, psychotherapy, such as cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), or dialectical behavior therapy (DBT), can help individuals learn coping skills, identify negative thought patterns, and address underlying emotional issues contributing to depression. Lifestyle changes, such as regular exercise, healthy eating, stress management, and social support, are also important components of depression treatment.
Conclusion
In conclusion, the science behind depression is complex and multifaceted, involving a combination of genetic, biological, psychological, and environmental factors. Neurochemical imbalances in the brain, including alterations in serotonin, dopamine, norepinephrine, and GABA function, play a significant role in the development and progression of depression. Understanding these neurochemical mechanisms can help inform more effective treatment approaches for individuals struggling with depression, ultimately improving outcomes and quality of life.
For additional resources on depression, pls visit here.
To read about 5 MYTHS ABOUT EATING DISORDERS YOU MUST STOP BELIEVING please click here.


1 thought on “The Science Behind Depression: Understanding Neurochemical Imbalances – Exclusive Report”